Pocket processor allows for zoom and brightness adjustment.
PRIMA Visual Prosthesis
Groundbreaking BCI Vision Restoration Technology
Translate
- English
- German (Deutsch)
PRIMA is a sophisticated system designed to replace the function of light sensitive cells in the eye that have been lost due to advanced degenerative retinal diseases.
Vision is the product of many layers of cells passing visual information into the brain. In degenerative retinal diseases, like age-related macular degeneration, the light-sensitive first layer of cells (rods and cones) fail, leading to blindness. By stimulating the next layer of cells (bipolar cells) directly, bypassing the lost rods and cones, visual input can be restored to the brain.
Our ongoing PRIMAvera clinical study is evaluating PRIMA for people with advanced atrophic dry age-related macular degeneration.
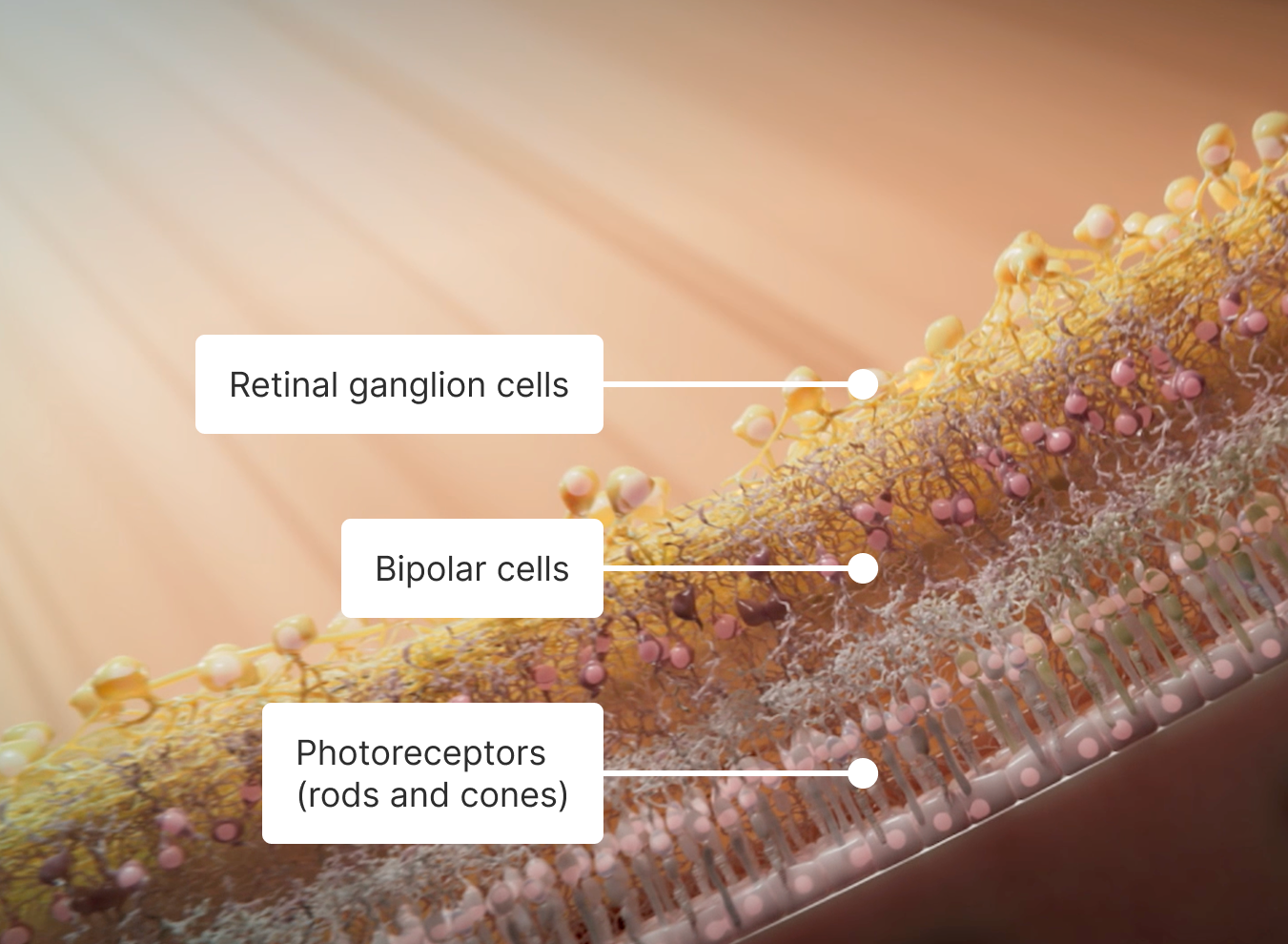
Science PRIMA bypasses lost photoreceptors and stimulates the remaining cells in the retina with two components.
A small light-powered implant placed under the retina, which is designed to replace the function of light-sensitive cells lost to disease.
A special pair of glasses with an embedded camera and infrared projector sends light signals to the implant, providing both power and data.
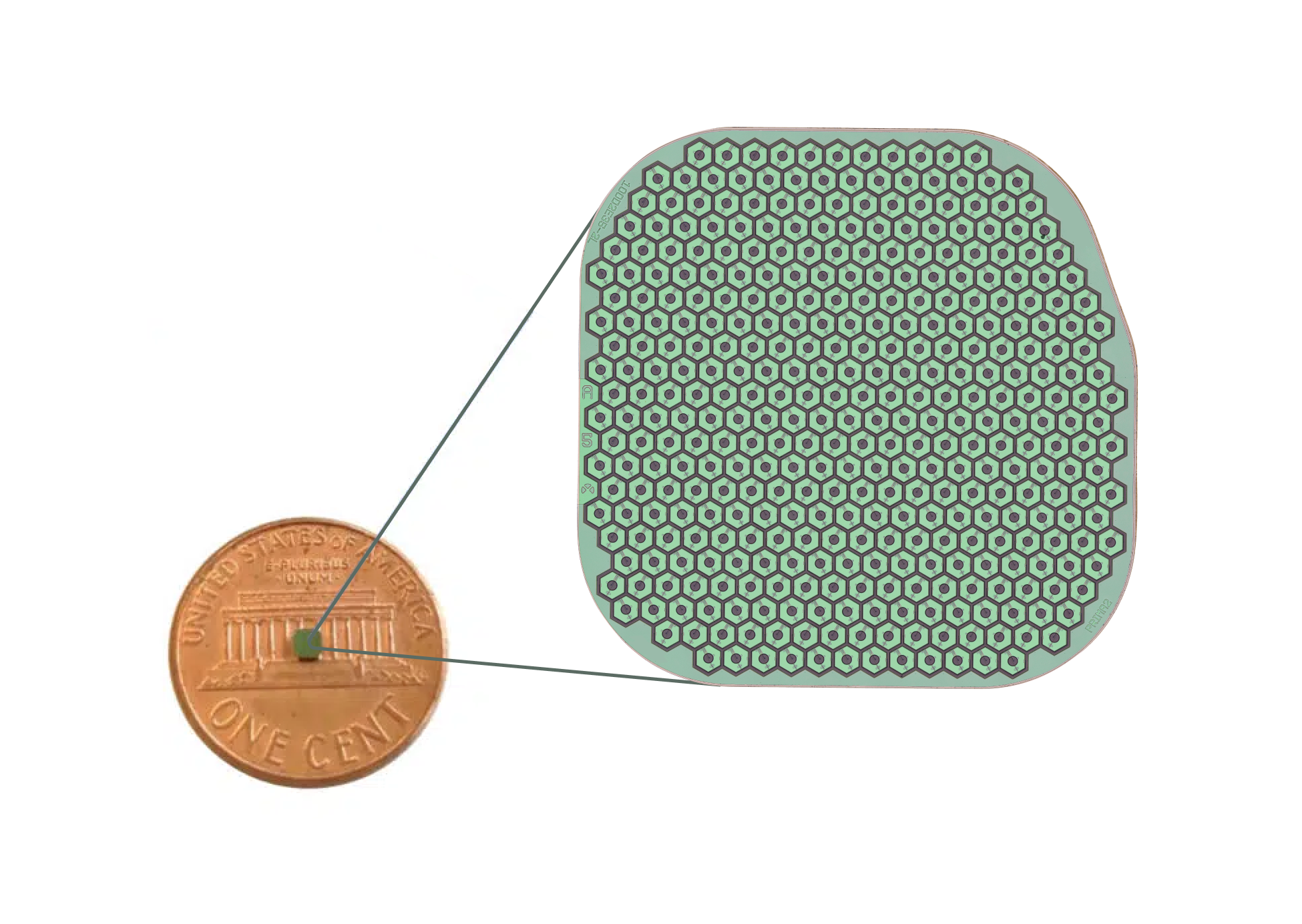
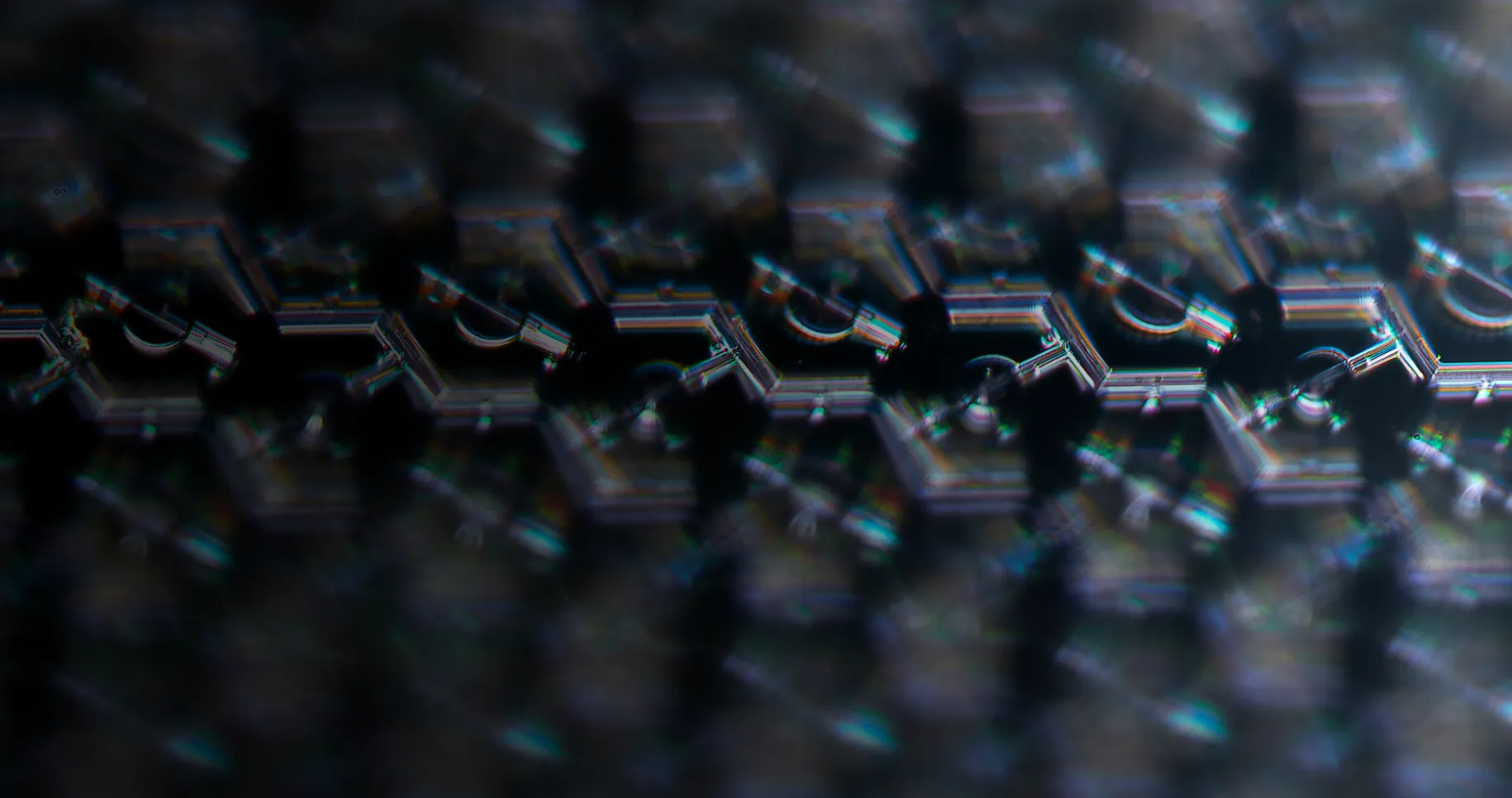
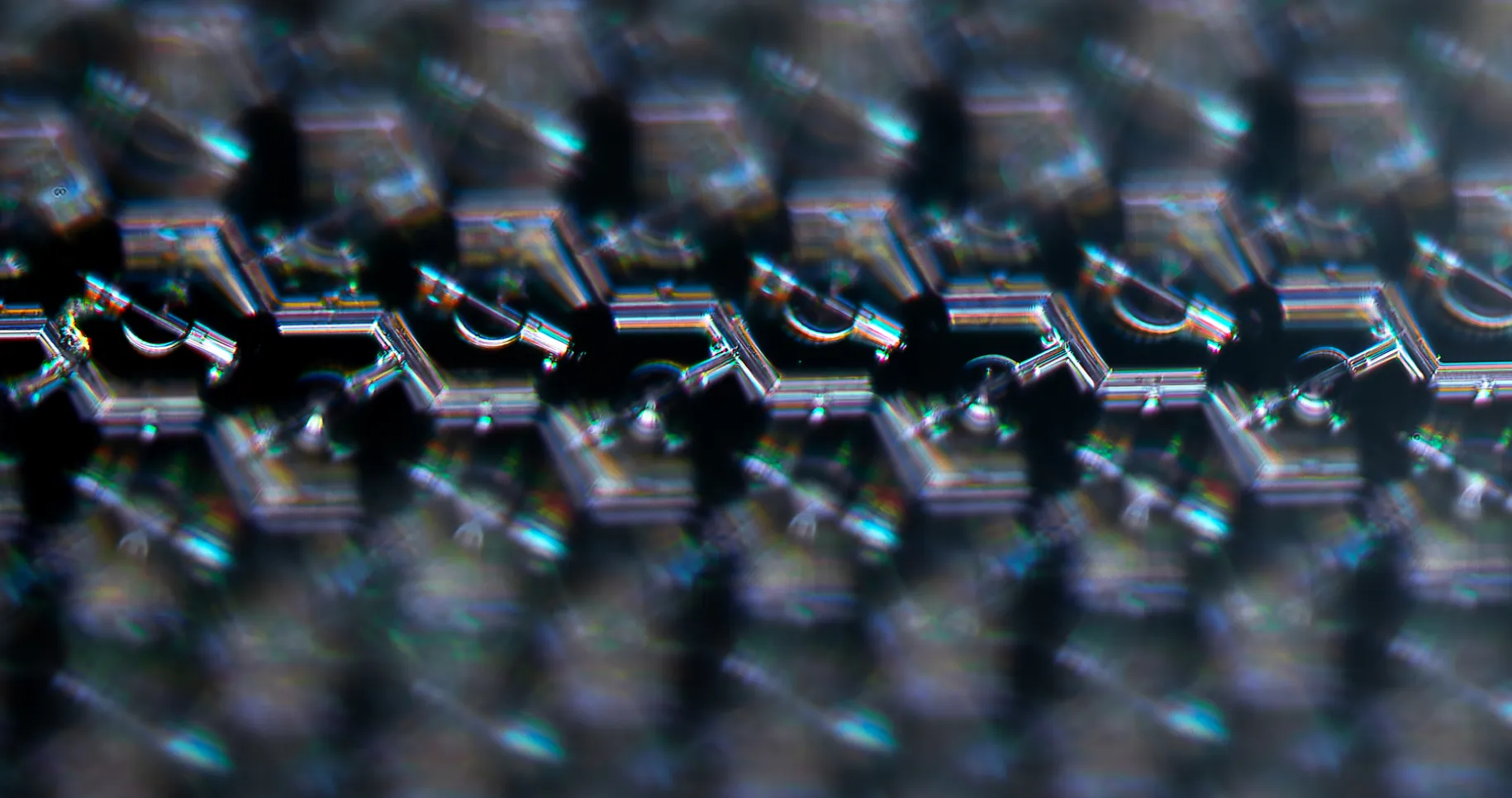
PRIMA Implant has 378 light-powered pixels
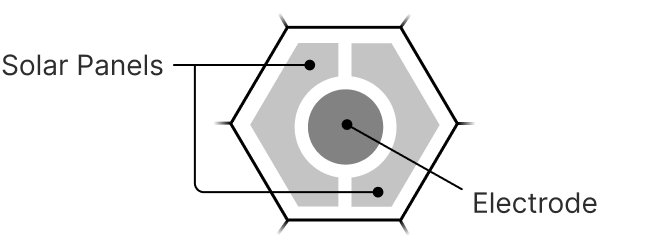
The implant has a honeycomb pattern of independently controlled pixels that convert infrared light, sent by a pair of glasses, into signals that activate neurons in the retina. When infrared light shines on a pixel it powers an electrode that stimulates the small part of the retina it is in direct contact with.
PRIMA Glasses use light to send power and information to the implanted device
These special glasses have a front-facing camera and an eye-facing infrared projector that shines light precisely on the PRIMA Implant. Only the pixels that the glasses illuminate are activated, providing PRIMA with both power and visual information.
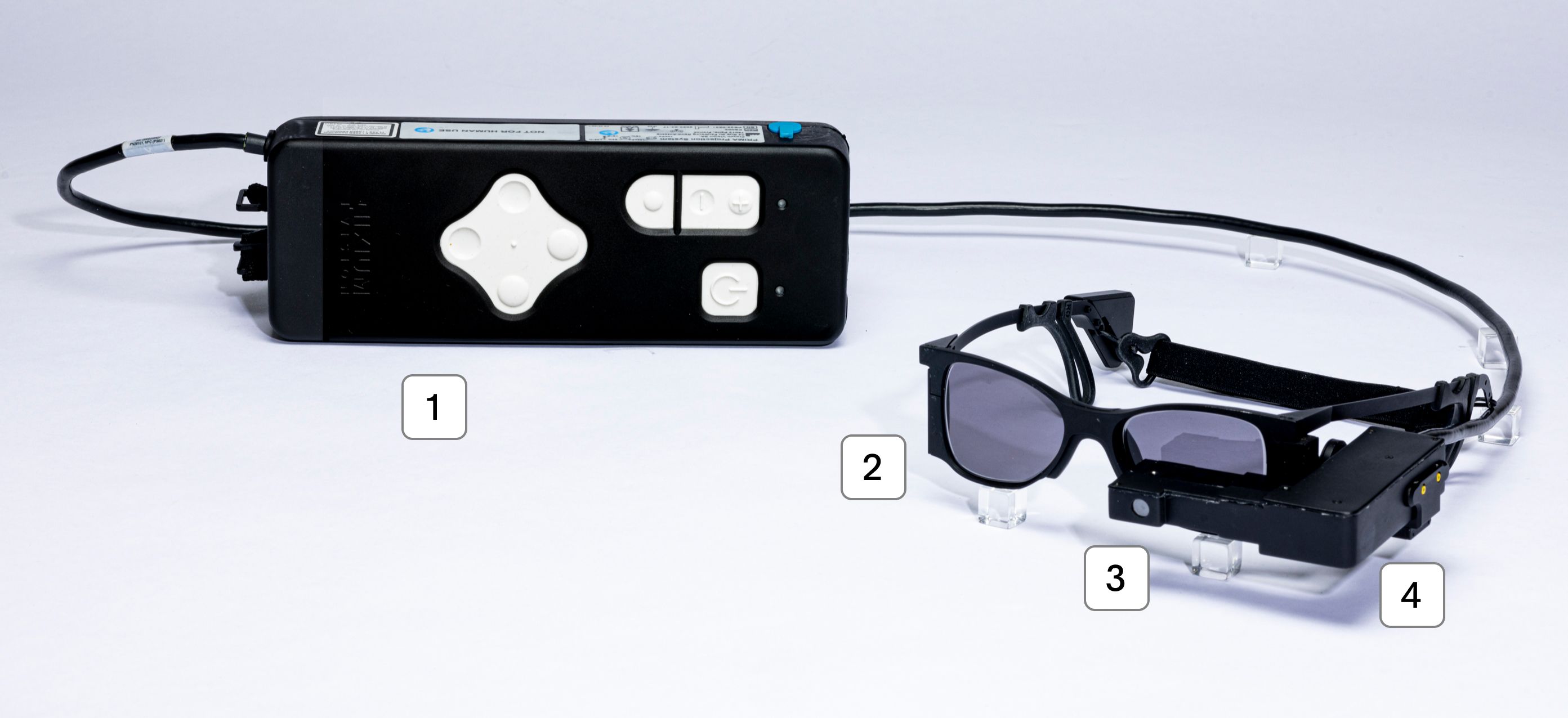
Sun lenses attenuate ambient light levels for optimal use.
Camera captures visual information.
Projection module sends patterns of infrared light into the eye.
This video shows how the PRIMA device is implanted and a simulation of what some may experience using the device.
Patient Registry: Science Corporation is actively seeking people interested in learning more about our vision loss treatments.
Join the Patient Registry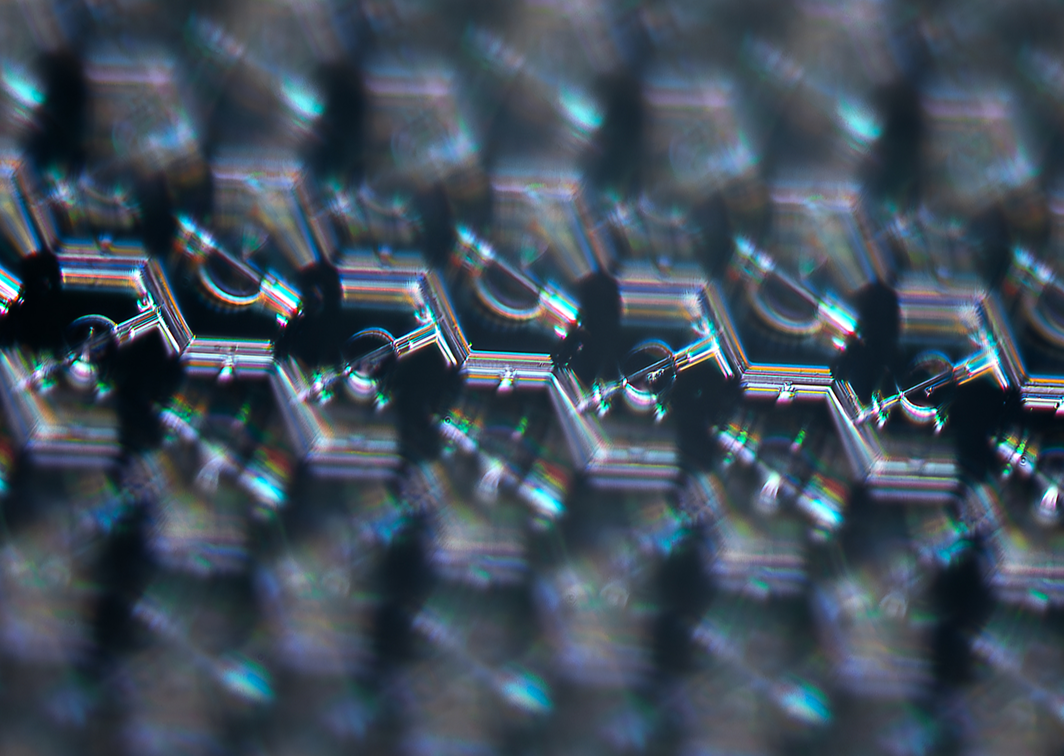
PRIMA Clinical Trials Status Tracker
In Progress : Macular Degeneration
Age-related macular degeneration (AMD) is a degenerative disease that causes a progressive loss of central vision.
Future Development : Retinitis Pigmentosa
Retinitis pigmentosa (RP) refers to a group of inherited diseases causing retinal degeneration and a loss of peripheral and night vision over time.
Future Development : Stargardt Disease
Stargardt disease is a genetic eye disorder that causes a progressive loss of central vision.
Science's PRIMAvera clinical study in Europe is indicated for advanced atrophic dry age-related macular degeneration (GA) (NCT04676854). The study is evaluating the safety and efficacy of the PRIMA implant for patients with AMD. Based on the positive preliminary results, we have submitted an application for a CE mark to the European Union.
A separate feasibility study in the US is ongoing. Results from the US study (NCT 03392324) and European study (NCT 03333954) measuring near visual acuity at months 12 and 24 post-implantation are available.
News & Updates
Related Scientific Publications
Read the research and scientific studies supporting the PRIMA system.
Subretinal Photovoltaic Implant to Restore Vision in Geographic Atrophy Due to AMD
Long-term observations of macular thickness after subretinal implantation of a photovoltaic prosthesis in patients with atrophic age-related macular degeneration
Simultaneous perception of prosthetic and natural vision in AMD patients
Photovoltaic Restoration of Central Vision in Atrophic Age-Related Macular Degeneration
Restoring sight with retinal prostheses
Optimization of pillar electrodes in subretinal prosthesis for enhanced proximity to target neurons
Join our Medical Professional Network
If you are a medical professional interested in learning more details about PRIMA's mechanism of action or the surgical implant technique, please consider joining our professional network.
Join our professional networkCAUTION: Investigational device. Limited by federal law to investigational use.
Hardware shown is for display purposes only. Actual device shape and color may vary.